As physiotherapy professionals, we understand that posture is the window to the musculoskeletal system. Among the various assessment tools available to us, the plumb line stands as one of the most fundamental yet powerful methods for evaluating postural alignment. This comprehensive guide explores every aspect of plumb line assessment, from its basic principles to advanced clinical applications, providing you with the knowledge needed to master this essential physiotherapy skill.
Understanding the Plumb Line: More Than Just a Vertical Reference
The plumb line is a simple yet sophisticated tool that represents the theoretical line of gravity passing through the human body in an upright stance. Named after the Latin word “plumbum” (lead), it consists of a weighted string or cord that, when suspended, creates a perfectly vertical reference line due to gravitational force. In physiotherapy practice, this vertical reference serves as our gold standard for assessing postural deviations and identifying musculoskeletal imbalances.
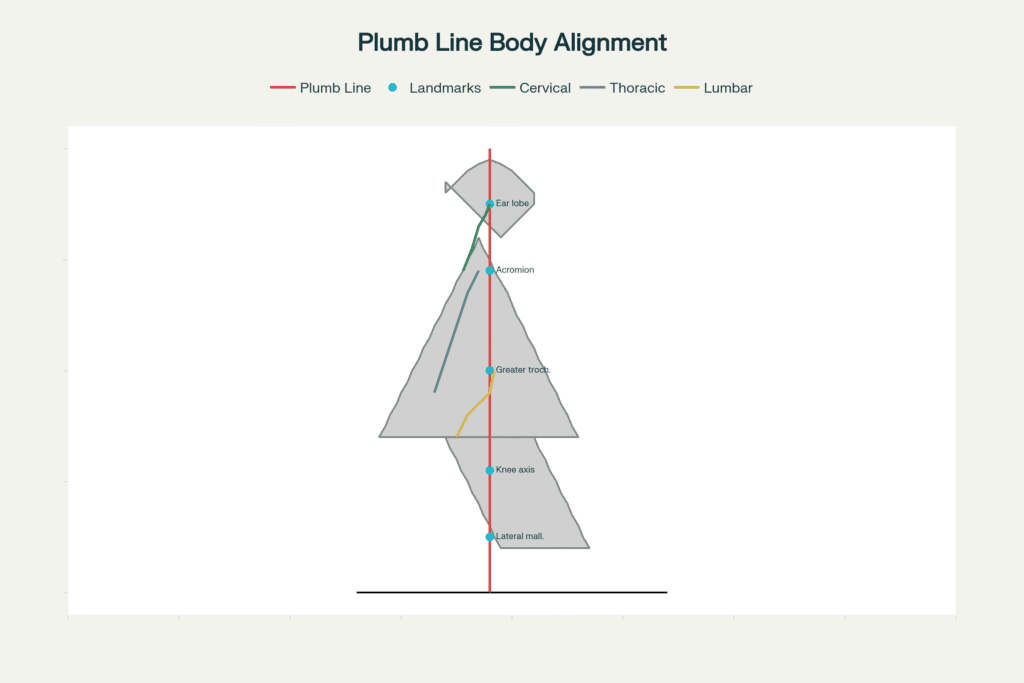
Ideal plumb line alignment showing anatomical landmarks for postural assessment in physiotherapy
What makes the plumb line particularly valuable in clinical practice is its direct relationship to the line of gravity – the vertical projection of the body’s center of mass to the ground. When a person exhibits ideal posture, specific anatomical landmarks should align with this vertical reference, creating optimal biomechanical efficiency and minimal energy expenditure for maintaining upright stance.
The Science Behind Line of Gravity and Body Mechanics
The relationship between posture and gravity is fundamental to human bipedalism. Research demonstrates that the human body’s center of gravity is located approximately at the second sacral vertebra (S2), about 55% of total height from the ground in women and 57% in men. This center of gravity must remain within the base of support created by the feet to maintain stable upright posture without excessive muscular effort.
The line of gravity represents the vertical projection of this center of mass, and any deviation from ideal alignment requires compensatory muscle activation to prevent falling. Studies using force plate analysis have shown that optimal postural alignment minimizes the work required by postural muscles, reducing fatigue and the risk of overuse injuries.
Modern biomechanical research has revealed that the line of gravity doesn’t pass through all joint centers simultaneously in most individuals, but the closer the alignment, the more efficient the postural system becomes. This understanding forms the scientific foundation for our clinical use of plumb line assessment.
Critical Anatomical Landmarks: Your Roadmap to Postural Assessment
Lateral View Assessment (Sagittal Plane)
When performing a lateral plumb line assessment, the following anatomical landmarks should align with or closely approximate the vertical reference line:
1. External Auditory Meatus (Ear Lobe)
The plumb line should pass through or very close to the ear lobe, indicating proper head positioning over the shoulders. Deviations suggest forward head posture or cervical spine dysfunction.
2. Acromion Process
The shoulder joint’s acromion process should align with the plumb line, representing balanced shoulder girdle positioning. Forward positioning indicates rounded shoulders and potential upper crossed syndrome.
3. Greater Trochanter
The line should pass through or slightly posterior to the greater trochanter of the femur, representing the hip joint axis. This landmark is crucial for assessing pelvic positioning and hip joint alignment.
4. Knee Joint Axis
The plumb line should pass slightly anterior to the transverse axis of the knee joint, creating a slight extension moment that helps maintain knee stability without excessive muscular effort.
5. Lateral Malleolus
The line should fall slightly anterior to the lateral malleolus of the ankle, typically through the calcaneocuboid joint. This positioning optimizes ankle strategy for postural control.
Spinal Alignment Considerations
The plumb line should pass through the bodies of the cervical and lumbar vertebrae, maintaining the natural spinal curves while ensuring balanced loading through the vertebral column.
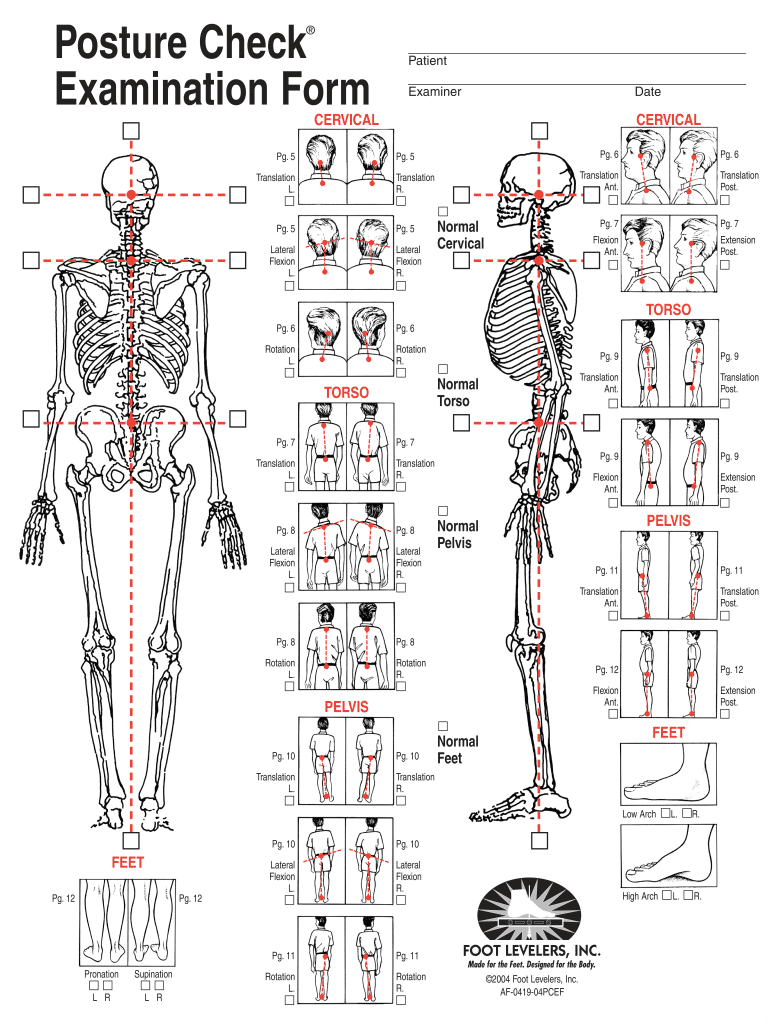
Posterior and Anterior View Assessment (Frontal Plane)
From the posterior view, the plumb line should bisect the body symmetrically, passing through the external occipital protuberance, cervical and lumbar spinous processes, and the gluteal cleft. Any lateral deviations may indicate scoliosis, pelvic asymmetries, or compensatory patterns.
Clinical Application: When, Where, and How to Use Plumb Line Assessment
When to Use Plumb Line Assessment
Primary Indications:
- Initial postural screening for new patients
- Monitoring postural changes throughout treatment
- Identifying compensation patterns in chronic pain patients
- Pre and post-intervention assessments
- Workplace ergonomic evaluations
- Sports performance optimization
Optimal Timing:
Research suggests that plumb line assessments should be performed when patients are in their natural, relaxed stance rather than artificially corrected posture. Allow patients to “settle” into their typical posture by having them walk in place or perform gentle movements before assessment.
Clinical Setting Requirements
Equipment Needed:
- Plumb line (weighted string or chain)
- Stable suspension point (ceiling mount or adjustable stand)
- Adequate lighting for clear visibility
- Camera for documentation (optional but recommended)
- Postural grid or measuring tape for quantification
Patient Preparation:
- Minimal clothing (shorts/sports bra for women, shorts for men)
- Removal of shoes and heavy jewelry
- Hair tied back to visualize cervical landmarks
- Explanation of procedure to reduce patient self-consciousness
Step-by-Step Assessment Protocol
1. Setup Phase
Position the plumb line approximately 30-50cm behind the patient for lateral view assessment. Ensure the weighted end stabilizes before beginning observation.
2. Patient Positioning
Instruct the patient to stand naturally, avoiding conscious postural correction. Use the “elevator waiting” instruction to encourage natural stance.
3. Assessment Sequence
- Begin with lateral view (both left and right sides)
- Progress to posterior view
- Complete with anterior view if indicated
- Document findings immediately
4. Measurement and Documentation
Measure deviations in millimeters or centimeters from the plumb line to specific anatomical landmarks. Research indicates that deviations greater than 10mm are clinically significant.
Common Postural Deviations: Recognition and Clinical Implications
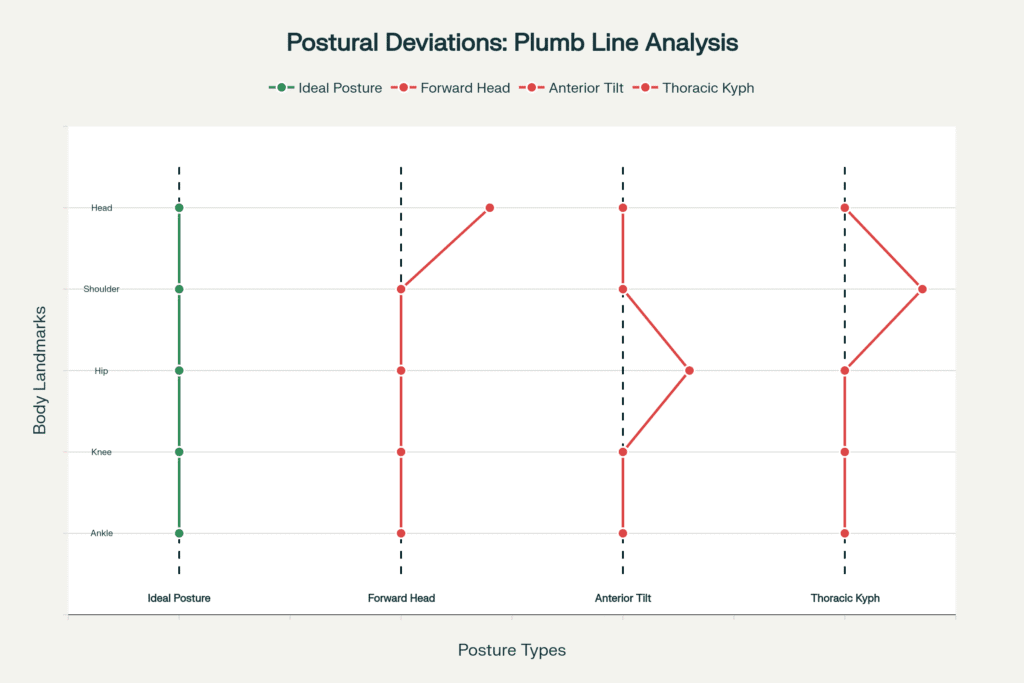
Forward Head Posture
Characteristics: Ear positioned anterior to the plumb line, often with loss of cervical lordosis
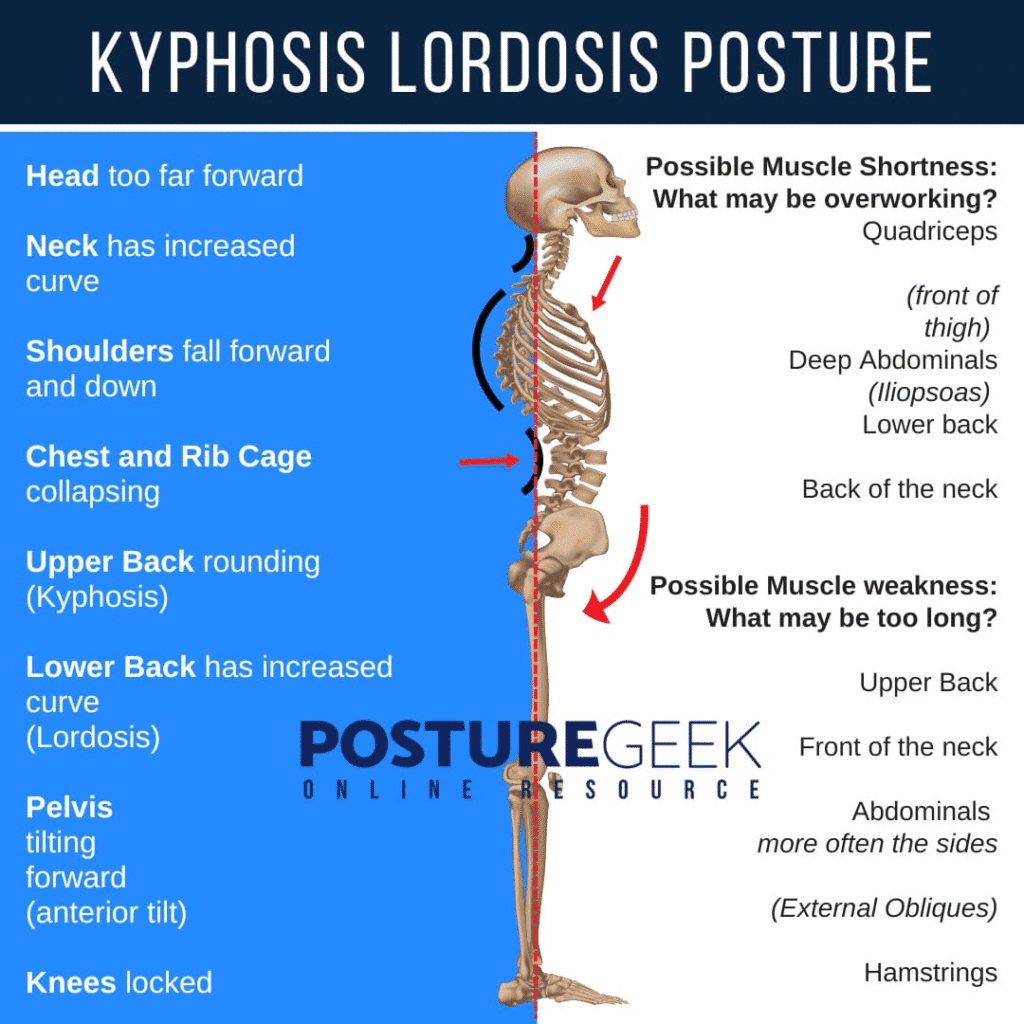
Lateral view skeleton showing kyphosis and lordosis postural deviations with muscle imbalance insights relevant to physiotherapy assessment.
Clinical Significance:
Associated with cervical pain, headaches, temporomandibular dysfunction, and upper crossed syndrome
Prevalence:
Estimated to affect up to 66% of the population, particularly those with desk-based occupations
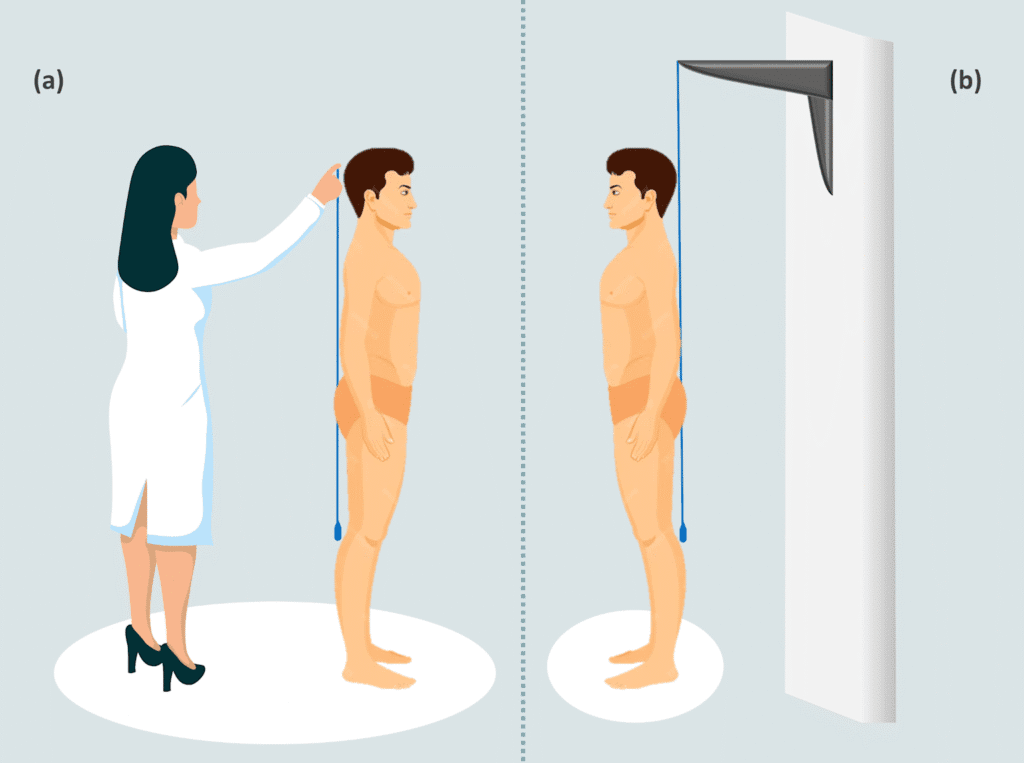
Illustration of plumb line use in physiotherapy postural assessment showing manual and fixed setups for evaluating body alignment.
Increased Thoracic Kyphosis
Characteristics: Excessive posterior curvature of the thoracic spine (>50°), with shoulders positioned anterior to the plumb line.
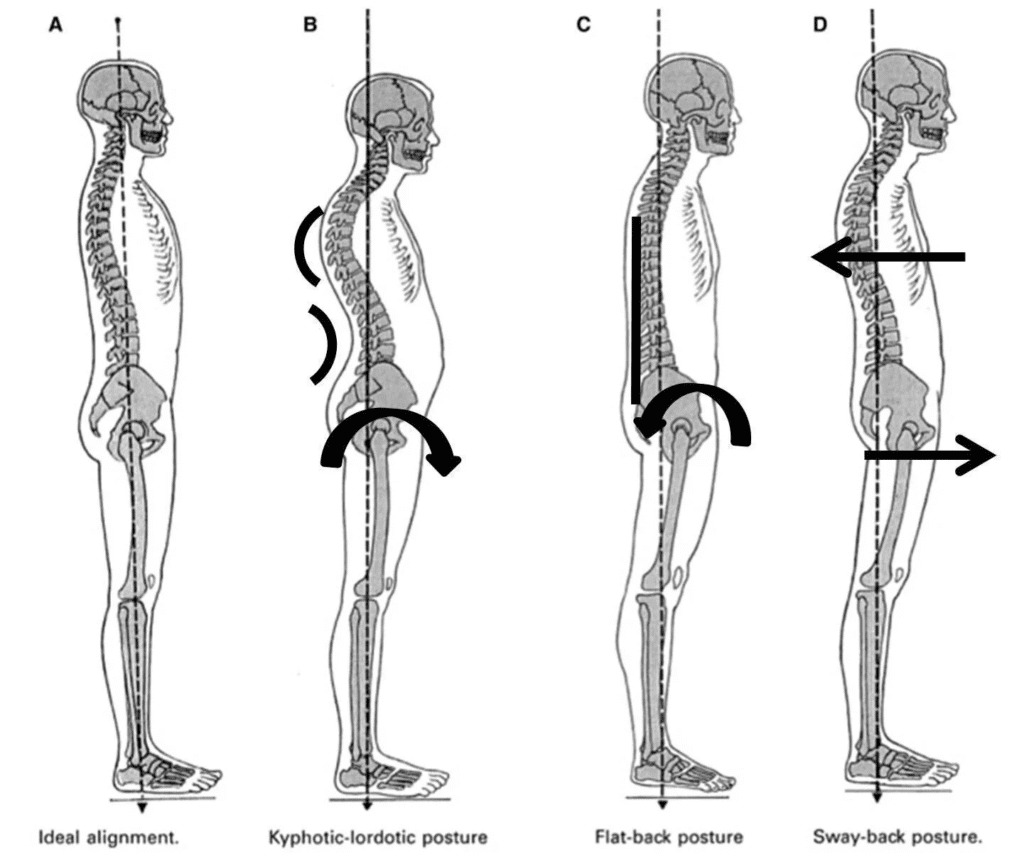
Illustration of ideal and common postural deviations using a plumb line to show body alignment changes relative to the line of gravity.
Clinical Implications: May compromise respiratory function, increase fall risk in elderly, and contribute to chronic back pain
Assessment Notes: Consider age-related changes and differentiate between structural and postural components
Anterior Pelvic Tilt and Lumbar Lordosis
Characteristics: Pelvis tilted forward with increased lumbar curve, often with hip positioned anterior to the plumb line
Associated Conditions: Lower back pain, hip flexor tightness, gluteal weakness, and lower crossed syndrome
Prevalence: Studies indicate this affects approximately 75% of women and 85% of men to varying degrees
Posterior Pelvic Tilt
Characteristics: Flattened lumbar curve with hip positioned posterior to normal alignment
Clinical Considerations: Often associated with tight hamstrings, weak hip flexors, and may indicate degenerative changes in older adults
Advanced Assessment Techniques and Modern Applications
Digital Enhancement and Technology Integration
Modern physiotherapy practice increasingly incorporates technology to enhance plumb line assessment accuracy. Photogrammetric analysis allows for precise measurement and longitudinal tracking of postural changes. Studies demonstrate excellent reliability (ICC > 0.90) when using digital photography combined with plumb line reference.
Smartphone Applications:
Recent research has validated several mobile applications for postural assessment, offering convenient alternatives to traditional plumb line methods while maintaining clinical accuracy.
Fixed Plumb Line Systems
Innovative approaches include fixed plumb line (FPL) systems that attach to walls or ceiling mounts, eliminating examiner variability and improving measurement precision. Research shows FPL systems demonstrate superior reliability compared to handheld methods, with intraclass correlation coefficients exceeding 0.94.
Reliability, Validity, and Clinical Limitations
Research Evidence for Reliability
Multiple studies confirm the reliability of plumb line assessment when performed by trained clinicians. Inter-rater reliability ranges from 0.70-0.85 for traditional methods, improving to >0.90 with standardized protocols and digital enhancement.
Generated File
Key Factors Affecting Reliability:
- Examiner training and experience
- Patient positioning consistency
- Environmental factors (lighting, distractions)
- Time of day (postural fatigue effects)
- Patient self-consciousness and compensation
Clinical Limitations and Considerations
Accuracy Limitations:
Research indicates that visual assessment of subtle postural deviations (<5mm) may be unreliable without technological assistance. The plumb line method works best for detecting moderate to significant deviations.
Population Considerations:
- Children and adolescents: Consider growth-related changes
- Elderly patients: Account for age-related postural changes
- Athletic populations: May have sport-specific adaptations
- Pregnancy: Temporary postural adaptations are normal
Contraindications:
- Acute pain conditions preventing comfortable standing
- Balance disorders requiring assistance
- Cognitive impairments affecting instruction comprehension
Integration with Comprehensive Postural Assessment
Complementary Assessment Methods
While plumb line assessment provides valuable static postural information, integration with other methods enhances clinical decision-making:
Movement Screening:
- Overhead squat assessment
- Single-leg stance testing
- Gait analysis
- Functional movement patterns
Quantitative Measurements:
- Goniometry for specific joint angles
- Inclinometry for spinal curvatures
- Photogrammetric analysis for precision
- 3D motion analysis for research applications
Clinical Decision Making
Plumb line findings should be interpreted within the context of:
- Patient symptoms and functional limitations
- Occupational and lifestyle factors
- Previous injury history
- Treatment goals and expectations
- Other examination findings
Therapeutic Implications and Treatment Planning
Evidence-Based Treatment Approaches
Research demonstrates that postural deviations identified through plumb line assessment respond well to targeted interventions:
Forward Head Posture Interventions:
- Deep cervical flexor strengthening
- Upper cervical extension exercises
- Postural awareness training
- Ergonomic modifications
Effectiveness: Studies show significant improvements in craniovertebral angle following 6-8 weeks of targeted exercise.
Anterior Pelvic Tilt Corrections:
- Hip flexor stretching
- Gluteal strengthening
- Core stabilization exercises
- Posterior pelvic tilt training
Clinical Outcomes: Research indicates 60-80% of patients achieve clinically significant improvements with consistent intervention.
Monitoring Treatment Progress
Plumb line reassessment provides objective measures of treatment effectiveness:
- Initial assessment establishes baseline
- 4-6 week intervals monitor progress
- Final assessment documents outcomes
- Long-term follow-up prevents regression
Professional Development and Best Practices
Enhancing Assessment Skills
Training Recommendations:
- Practice on diverse populations
- Participate in inter-rater reliability studies
- Attend continuing education workshops
- Integrate technology when available
Documentation Standards:
- Use standardized measurement protocols
- Photograph findings when possible
- Quantify deviations in measurable units
- Track changes over time
Ethical Considerations
Patient Comfort and Dignity:
- Ensure appropriate draping and privacy
- Explain the assessment purpose clearly
- Respect cultural sensitivities
- Obtain informed consent for photography
Future Directions and Emerging Technologies
Artificial Intelligence Integration
Emerging technologies show promise for automated postural analysis using AI algorithms to identify deviations from plumb line references. These systems may enhance accuracy while reducing assessment time.
Wearable Technology
Research into wearable postural monitoring devices offers potential for continuous assessment and real-time feedback, extending beyond clinical settings into daily life monitoring.
Virtual Reality Applications
VR-based postural training programs show preliminary promise for enhancing postural awareness and correction, potentially revolutionizing rehabilitation approaches.
Conclusion: Mastering the Art and Science of Plumb Line Assessment
The plumb line remains an indispensable tool in the physiotherapist’s assessment arsenal, bridging the gap between simple observation and sophisticated biomechanical analysis. Its enduring value lies not merely in its simplicity, but in its direct relationship to fundamental principles of human posture and movement.
As we’ve explored throughout this comprehensive guide, successful plumb line assessment requires more than just hanging a string and observing deviations. It demands a deep understanding of biomechanics, anatomy, and the complex interplay of factors that influence human posture. The integration of traditional techniques with modern technology offers unprecedented opportunities for precision and patient engagement.
Key Takeaways for Clinical Practice:
The plumb line assessment serves as both a diagnostic tool and an educational resource, helping patients visualize their postural patterns while providing physiotherapists with objective data for treatment planning. When performed correctly and interpreted within appropriate clinical context, it remains one of our most valuable methods for understanding and addressing postural dysfunction.
Remember that postural assessment is not merely about achieving perfect alignment – it’s about optimizing function, reducing pain, and enhancing quality of life. The plumb line serves as our guide in this endeavor, helping us navigate the complex relationship between structure and function in the human body.
As you continue to develop your skills in postural assessment, embrace both the traditional foundations and emerging innovations in the field. The future of physiotherapy lies in our ability to combine time-tested methods like plumb line assessment with cutting-edge technology, creating more effective and engaging treatment approaches for our patients.
Through mastery of plumb line assessment, we equip ourselves with a fundamental skill that enhances our ability to help patients achieve optimal postural health and functional movement. This foundation serves not only our current practice but prepares us for the evolving landscape of physiotherapy assessment and intervention.
Ready for Your Free Posture Breakthrough?
Discover how our Evidence-Based Plumb Line Assessment uncovers the real reasons behind your pain—and unlocks a customized recovery journey that clinics don’t want you to know.
Click below for your Free First Session—meet our expert team, experience your personalized assessment, and see how small adjustments can transform your comfort and confidence in daily life.